Illinois panel targets Medicare fraud
By Kevin Beese Staff Reporter — December 18, 2018
Bradley Hart, inspector general at the Department of Healthcare and Family Services, talks about Medicaid abuse. “Illinois’ most vulnerable citizens lose out on critical health-care services when criminals take advantage of the state’s Medicaid system,” Hart said. (BlueRoomStream.com)
Illinois’ most strapped residents are the one who wind up paying when Medicare fraud takes place, according to Gov. Bruce Rauner.
The governor said it is estimated that $1 billion in unwarranted Medicare payments have been made, costing taxpayers “extra money and it hurts health-care services to our most vulnerable residents who deserve to get proper health-care support.”
In its latest report, the Governor’s Health Care Fraud Elimination Task Force showed that it successfully avoided or recouped $218 million in wasteful or fraudulent Medicaid spending. The effort resulted in 39 fraud convictions including $27.8 million in recoveries through criminal prosecutions, civil actions and/or administrative referrals. The state Department of Healthcare and Family Services Office of Inspector General saved or recouped an estimated $190 million in Fiscal Year 2018. The Task Force has saved the state more than $665 million since its inception in 2016, Rauner said.
“The state of Illinois dedicates a tremendous amount of resources to health-care programs, and it is our responsibility to make sure those taxpayer dollars are spent on care instead of lining criminals’ pockets,” Rauner said at a Dec. 12 press conference. “The Health Care Fraud Elimination Task Force plays a crucial role in ensuring that state dollars are distributed both efficiently and fairly.”
Chaired by Executive Inspector General Susan Haling, the Task Force’s purpose is to develop and coordinate a plan to prevent and eliminate health-care fraud, waste and abuse by deploying a cross-agency, data-driven approach. The Task Force specifically focuses on reducing wasteful spending and fraud in Medicaid, Worker’s Compensation, and state employee group insurance.
“Health-care fraud is an enormous problem in Illinois, and I am very proud of the Task Force’s efforts to eliminate fraud in the state,” Haling said. “While there is much work to be done still, the Task Force has demonstrated that cooperation between government agencies produces results.”
The Task Force has worked with a variety of stakeholders to achieve the results described in its report.
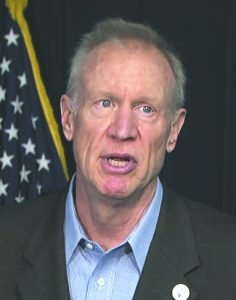
Gov. Bruce Rauner talks at a Dec. 12 press conference about steps the state has taken to stop Medicare fraud. Illinois has avoided or recouped $218 million in wasteful or fraudulent Medicare spending. (BlueRoomStream.com)
In FY 2017, members of the Task Force participated in the 2018 National Health Care Fraud Takedown, which was the largest health-care fraud enforcement action in U.S. Department of Justice history. The Illinois State Police Medicaid Fraud Control Unit’s participation led to the indictment of 14 people responsible for $430,000 in fraudulent claims in the Medicaid Home Services Program. Task Force members also participated in the U.S. Attorney’s Office Health Care Fraud Task Force meetings to share information about data-driven approaches to fighting fraud.
The state’s Healthcare and Family Services Office of the Inspector General also rolled out a program that provides hospitals with the opportunity to self-audit overpayments and billing errors. Piloted in 2016, the program resulted in the identification of $4.4 million in overpayments.
“By working together with health-care providers and the U.S. Department of Justice, the Health Care Fraud Elimination Task Force ensures that state funds are used responsibly,” Rauner said.
Rauner added that the Task Force’s work is reflective of his administration’s emphasis on making state agencies more effective and efficient.
“My administration has prioritized modernizing state government operations,” Rauner said. “Collaboration and information sharing delivers value to Illinoisans by reducing costs and improving the quality of government services.”
The Task Force include: Deputy Gov. Trey Childress; Deputy General Counsel and Chief Compliance Officer Jill Hutchison; Jean Bohnhoff. director at the Department on Aging; Tim McDevitt, director at the Department of Central Management Services; Patricia Bellock, director at the Department of Healthcare and Family Services; James Dimas, director at the Department of Human Services; Kirk Lonbom, director at the Department of Innovation Technology; Jennifer Hammer, director at the Illinois Department of Insurance; Lt. David Roll at the Illinois State Police Medicaid Fraud Control Unit; Joann Fratianni at the Workers’ Compensation Commission; and Inspector General Bradley Hart at Healthcare and Family Services.
“The Illinois State Police Medicaid Fraud Control Bureau is honored to be part of this worthwhile initiative,” Roll said. “This initiative has served to enhance the cooperative efforts of all the involved agencies who are committed to combating fraud, waste and abuse of the Medicaid program in the state of Illinois.”
“In Fiscal Year 2018, our Home Services Program was able to recover more than $1.6 million in fraudulent payments, mostly through the implementation of an Electronic Visit Verification System. Modernizing our timekeeping system not only saves taxpayer dollars, but it also ensures our customers with disabilities are receiving the in-home care they need to stay safe and healthy,” said Dimas of Human Services. “We plan to duplicate this modernized timekeeping model in other IDHS program areas, making timekeeping for providers faster, easier and more accurate.”
“Illinois’ most vulnerable citizens lose out on critical health-care services when criminals take advantage of the state’s Medicaid system,” Hart said. “We’ve been aggressive in our efforts to crack down on fraud, abuse and mismanagement and we’ll continue to build resources and enhance our fraud fighting capabilities in order to protect Illinois taxpayers.”
kbeese@chronicleillinois.com



