Events put spotlight on Medicare fraud
By Kevin Beese Staff Writer — May 28, 2024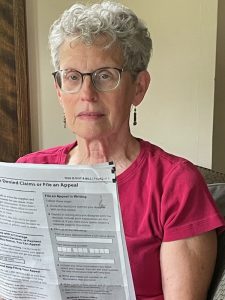
Linda Hennis of Oak Park holds the Medicare Summary that showed she had been billed $1,550 a month for catheters she never used. Events during Medicare Fraud Week, which is June 3-9, aim to raise awareness of fraud issues. (Provided photos)
Linda Hennis has never been catheterized, so she was more than a bit surprised to see that she had been billed for 200 intermediate catheters.
“I thought it was an error,” the Oak Park resident said upon checking her Medicare Summary report at the beginning of this year.
She started doing research and found that Medicare had been billed not only for the catheters in October, but $1,550 monthly for catheters from January to October 2023.
Her research tracked the catheter distribution to Pretty in Pink Boutique in El Paso, Texas.
“If I was to order catheters, why would I order them from El Paso, Texas?” Hennis asked.
The Oak Park resident never paid anything out of pocket for the catheters but learned that Medicare had paid $12,152 for the catheters she never got.
Medicare fraud is a huge problem nationally, according to Travis Trumitch, director of the Illinois Senior Medicare Patrol at AgeOptions, which coordinates community-based senior service agencies.
“No one wants to talk about it,” Trumitch said, “but there are a lot of case pending.”

Travis Trumitch
AgeOptions, the Area Agency on Aging of Suburban Cook County and Senior Medicare Patrol are ramping up efforts to educate older adults and people with disabilities during Medicare Fraud Prevention Week, which is June 3-9.
With most individuals qualifying for Medicare at age 65, the initiative aims to protect against fraud and ensure financial security.
AgeOptions is spearheading three events during Fraud Prevention Week to support older adults and caregivers, highlighted by the Fraud Fair Shred Event from 10 a.m. to 1 p.m. Thursday, June 6 at the Levy Senior Center in Chicago.
Other events are Senior Medicare Patrol Bingo on Tuesday, June 4 in Oak Forest and a Spanish SMP event Wednesday, June 5 at the Consulado General de Mexico in Chicago.
Linda Hennis has Medigap through Mutual of Omaha to pick up the health care costs that Medicare doesn’t. She said Mutual of Omaha didn’t pay for the catheters.
“They are very stringent on what they approve,” Hennis said.
A representative told her that when something odd comes through like 200 catheters in a month, the company requests more information and the patient’s medical records.
“It is a cash cow,” Hennis said of Medicare fraud.
A post on the website of Pretty in Pink Boutique, a Christian-based ministry for women and their families in the journey with breast cancer, notes that the agency is not the one that submitted catheter claims with Medicare.
“We have received dozens of calls from people who received fraudulent claims made by Pretty in Pink Boutique, Inc. While we share the same name, this company is completely unaffiliated with us,” the post reads. “There are at least five companies registered with Medicare that operate with the name Pretty in Pink Boutique.
“We have reported the calls we are receiving to Medicare, and we have been working with callers to try to figure out exactly who is filing these claims so that we can communicate anything we know to Medicare. Fraudulent claims are bad for all of us and we are on your side.
“We are not even set up to bill catheters (which is the most common item we’ve seen on these claims) and the claims we’ve been able to review contain an entirely different Medicare Identification Number from ours. You’ll also notice our website doesn’t mention anything about catheters. We only bill for mastectomy supplies and compression garments.”
AgeOption’s Travis Trumitch said the three biggest Medicare scams being seen right now in Illinois are urinary track catheters, durable medical equipment such as braces, and genetic testing.
In the durable equipment scam, a “Medicare call center” contacts a senior and asks if he or she would like a free brace. In a data breach, the senior provides identity information.
“If they send a brace at all, it doesn’t fit or is the wrong item,” Trumitch said. “That’s a big problem because the person may have been charged for a brace in 2018 and thrown it in the closet because it didn’t fit. Now in 2024, the person needs a brace and Medicare is not going to pay because it already paid for one.”
In the genetic testing scams, individuals posing as affiliates of genetic research firms, swap seniors’ mouths and then submit the swaps to Medicare as $12,000 cancer screenings.
“The senior’s DNA is stolen and if they get any genetic results at all, there is little information and nobody to explain the results to them,” Trumitch said.
Trumitch said the genetic testing scams was happening pre-pandemic and is now returning.
“Fraudsters are good about waiting and coming back with something,” he said.
Spreading information about Medicare fraud is vital, Trumitch said.
“Educating Illinois’ older adult population about the dangers of Medicare fraud is essential,” said Trumitch. “Events such as the Fraud Fair empower these individuals along with their providers and caretakers to defend against scams and fraudulent activities aimed at Medicare beneficiaries, ensuring their access to essential health care services.”
Linda Hennis, a former nurse, said Medicare fraud must be stopped.
“To think that we have to pay higher Medicare premiums or that Medicare might run short because of this is wrong,” Hennis said. “We need this money.”
The Oak Park resident said individuals don’t need medical experience to peruse their Medicare summary.
“You don’t need any specialized training to figure out the Medicare Summary,” Hennis said. “Look at it. If it’s all been paid, don’t stop there. Take a quick glance at the lab work, the service providers. Make sure it adds up.”
Learn about Medicare fraud and events during Medicare Fraud Prevention Week at www.smpresource.org.
kbeese@chronicleillinois.com







