Loss of rural health services creating care deserts
By Tammie Sloup FarmWeek — February 24, 2022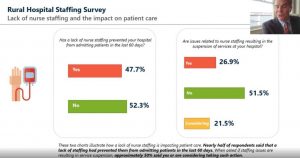
While pandemic funding has provided temporary stabilization to rural hospitals, the emerging nursing shortage continues to worsen, according to Michael Topchik, national leader of The Chartis Center for Rural Health. (Photo by Tammie Sloup of FarmWeek)
A rural health care advisory and analytics provider has found nearly half of rural hospitals have refrained from admissions because of nursing shortages this past year.
Additionally, more than a quarter of rural hospitals have ceased offering some services due to staffing challenges.
“Alarm bells should be ringing on this topic. This is a very big deal,” said Michael Topchik, the national leader of The Chartis Center for Rural Health, during the National Rural Health Association’s Policy Institute on Feb. 8.
Utilizing analytics and data to understand and address issues challenging the rural health safety net including health disparities and inequity, provider vulnerability and sustainable performance improvement, Topchik said that while pandemic funding has provided temporary stabilization to rural hospitals, the emerging nursing shortage continues to worsen.
“This is the No. 1 need in our surveys and across a variety of ways we’ve looked at this, this is the biggest challenge rural hospitals tell us they have is staffing, staffing, staffing,” Topchik said.
The majority of nurses who have left rural hospitals exited for more lucrative positions, while others report being burned out from the pandemic and having to cover as a result of shortages.
Staffing shortages have also impacted services. While some services were suspended by law during the pandemic, Chartis data highlighted trends with obstetric and chemotherapy services, which did not fall under that umbrella.
Between 2011 and 2021, 198 rural hospitals ceased to provide obstetrics, while 311 rural hospitals ceased to provide chemotherapy between 2014 and 2017.

Michael Topchik, national leader of The Chartis Center for Rural Health. (NRHA Twitter photo)
“I’m afraid to say that it’s really the story behind the story of the hospital closure crisis. It’s the story behind the story of the pandemic, which is that we’re seeing the loss of these services in rural areas, creating virtual deserts of care for very important services,” Topchik said.
Nearly half of rural hospitals are operating with a negative margin (excluding relief funds), with two rural hospitals closing in 2021, he said. The $12.6 billion in pandemic relief payments has helped, but only temporarily. And Topchik anticipates relative stability through 2022.
“There’s been some bright news, which is last year we didn’t see that many closures and we are predicting this year we won’t see that many either,” he said.
Attendees of the policy institute also met with members of Congress — including a handful from Illinois — to discuss emerging issues facing rural communities.
Following his meeting with Illinois rural health representatives, Sen. Dick Durbin, D-Springfield, issued a news release about the discussion in which he highlighted the $1 billion secured in the American Rescue Plan for the National Health Service Corps and Nurse Corps to build a more diverse pipeline of clinicians and recruit more health providers to serve in shortage areas.
To address other rural health care workforce issues, Durbin has introduced the bipartisan Rural America Health Corps Act, which would create a National Health Service Corps pilot program to test whether an expanded loan repayment award and service commitment — $200,000 over five years — would improve retention in rural communities, according to the news release.
The Chartis Group also announced the 2022 Top 100 Critical Access Hospitals and the 2022 Top 100 Rural & Community Hospitals. Based on the results of the Chartis Rural Hospital Performance INDEX, this annual recognition program honors outstanding performance among the nation’s rural hospitals.
A handful of Illinois hospitals made the lists, including Wabash General Hospital in Mount Carmel (critical access hospital); and HSHS St. Joseph’s Hospital in Breese, Jersey Community Hospital in Jerseyville and OSF Saint Elizabeth Medical Center in Ottawa (rural and community hospitals).
This story was distributed through a cooperative project between Illinois Farm Bureau and the Illinois Press Association. For more food and farming news, visit FarmWeekNow.com.







